Expanding global mental health and psychosocial support access
Most people around the world who are in need of mental health treatment or support are not able to access it. If you are interested in learning about scalable mental health and psychosocial support (MHPSS) interventions and approaches, contact us for quality-assured capacity strengthening in scalable psychological interventions tailored to meet your needs.
Photo: Trainers Teresa Ngigi and Lubos Tibensky at an SOS CV Italy training on EASE, hosted by University of Verona
MHPSS Academy
We envision a world where mental health support and psychosocial support is accessible to all through scalable interventions and approaches that can help to close the global mental health treatment gap. Capacity is not simply given, but strengthened together through mutual learning and respect for diverse knowledge. Our mission is to improve worldwide access to quality-assured capacity strengthening in scalable MHPSS interventions and approaches for individuals and organizations – centering collaboration and a shared commitment to accessible mental health support.










Scalable MHPSS interventions improve mental health and psychosocial well-being by efficiently reaching large numbers of individuals through accessible, cost-effective approaches. These brief, non-specialist-delivered versions of evidence-based psychological treatments are modified to be delivered by non-specialists, as self-help interventions, or through digital platforms.
Scaling up access to MHPSS involves strengthening competencies of trainers who can then build skills in others to deliver these interventions. Join our Training of Trainers workshops or contact us for a tailored capacity-strengthening program designed to meet your specific needs.
photo: Koç University, Istanbul
MHPSS Academy
A number of scalable MHPSS interventions and approaches have been developed and are in use throughout the world. Some examples are:
Problem Management Plus (PM+)
Problem Management Plus (PM+) is a brief individual or group intervention designed to address psychological or social problems through problem-solving and behavioural interventions. It is delivered through five sessions where participants learn skills to manage stress, solve problems, get active, and strengthen their social support.
Read more here:
PROBLEM MANAGEMENT PLUS (PM+) Individual psychological help for adults impaired by distress in communities exposed to adversity https://iris.who.int/bitstream/handle/10665/206417/WHO_MSD_MER_16.2_eng.pdf?sequence=1
Scaling Up Psychological Interventions with Syrian Refugees (STRENGTHS) (http://strengths-project.eu/en/strengths-home/)
Refugee Minors and Integration (REMAIN) (https://ki.se/en/cns/remain-refugee-minors-and-integration)
RESPOND Project (https://respond-project.eu/)
Ukraine’s displaced people in the EU: Reach out, Implement, Scale-up and Evaluate interventions promoting mental wellbeing (U-RISE) (https://research.vu.nl/en/projects/ukraines-displaced-people-in-the-eu-reach-out-implement-scale-up-)
Building Mental Health and Psychosocial Support Capacity During a Pandemic: The Process of Adapting Problem Management Plus for Remote Training and Implementation During COVID-19 in New York City, Europe and East Africa (https://journals.lww.com/invn/fulltext/2021/19010/building_mental_health_and_psychosocial_support.6.aspx)
After the Randomised Controlled Trial Implementing Problem Management Plus Through Humanitarian Agencies – Three Case Studies from Ethiopia, Syria and Honduras (https://journals.lww.com/invn/fulltext/2021/19010/after_the_randomised_controlled_trial_.11.aspx)
Living Six Hours Away from Mental Health Specialists: Enabling Access to Psychosocial Mental Health Services Through the Implementation of Problem Management Plus Delivered by Community Health Workers in Rural Chiapas, Mexico (https://journals.lww.com/invn/fulltext/2021/19010/living_six_hours_away_from_mental_health.10.aspx)
Friendship Bench

Friendship Bench provides sustainable community based psychological interventions that are evidence based, accessible and scalable. Community health workers are trained to provide basic Cognitive Behavioural Therapy with an emphasis on Problem Solving Therapy, activity scheduling, and peer-led group support at primary care level. The mission of the Friendship Bench is to get people out of depression by creating safe spaces and a sense of belonging in communities, to enhance mental wellbeing and improve peoples’ quality of life. Guided by the values of empathy and connection and anchored in over a decade of rigorous research, Friendship Bench has re-imagined the delivery of evidence-based mental healthcare.
Read more here:
Friendship Bench Zimbabwe Website (https://www.friendshipbenchzimbabwe.org/)
Effect of a Primary Care–Based Psychological Intervention on Symptoms of Common Mental Disorders in Zimbabwe (https://jamanetwork.com/journals/jama/fullarticle/2594719)
Applying the Consolidated Framework for Implementation Research to Optimize Implementation Strategies for the Friendship Bench Psychological Intervention in Zimbabwe (https://link.springer.com/article/10.1007/s43477-023-00093-4)
Using the RE-AIM framework to evaluate the implementation of scaling-up the Friendship Bench in Zimbabwe – a quantitative observational study (https://doi.org/10.1186/s12913-022-08767-9)
Adaptation of a Problem-solving Program (Friendship Bench) to Treat Common Mental Disorders Among People Living With HIV and AIDS and on Methadone Maintenance Treatment in Vietnam: Formative Study (https://pubmed.ncbi.nlm.nih.gov/35802402/)
Group Interpersonal Therapy (IPT-G)
Group Interpersonal Therapy (IPT-G) is a form of psychotherapy that focuses on improving interpersonal relationships and addressing interpersonal issues within a group setting. It is a time-limited and structured therapeutic approach derived from Individual Interpersonal Therapy (IPT). The goal of IPT-G is to help individuals enhance their communication skills, manage conflicts, and develop healthier relationships with others.
Read more here:
Group Interpersonal Therapy (IPT) for Depression (https://iris.who.int/bitstream/handle/10665/250219/WHO-MSD-MER-16.4-eng.pdf?sequence=1)
Acceptability and impact of group interpersonal therapy (IPT-G) on Kenyan adolescent mothers living with human immunodeficiency virus (HIV): A qualitative analysis (https://bmcwomenshealth.biomedcentral.com/articles/10.1186/s12905-022-01807-w)
Culturally and developmentally adapting group interpersonal therapy for adolescents with depression in rural Nepal (https://bmcpsychology.biomedcentral.com/articles/10.1186/s40359-020-00452-y)
Group Problem Management Plus (Group PM+)
Learn more about PM+ with our information leaflet
Problem Management Plus for Groups (Group PM+) is a psychological intervention to provide mental health support in communities affected by adversity adapted from the individual-focused Problem Management Plus (PM+) intervention.
Read more here:
Group Problem Management Plus (Group PM+): group psychological help for adults impaired by distress in communities exposed to adversity (https://www.who.int/publications/i/item/9789240008106)
Effectiveness of Group Problem Management Plus, a brief psychological intervention for adults affected by humanitarian disasters in Nepal: A cluster randomized controlled trial (https://journals.plos.org/plosmedicine/article?id=10.1371/journal.pmed.1003621)
Thinking Healthy
Thinking Healthy is a program and intervention developed to address prenatal depression. The program is designed to provide support and improve mental health outcomes for pregnant women and new mothers. Grounded in evidence-based cognitive behavioral techniques that are recommended by the WHO’s mhGAP program, the goal of the Thinking Healthy program is to improve maternal mental health, enhance the mother-infant relationship, and contribute to overall family well-being.
Read more here:
Thinking Healthy: A manual for psychological management of perinatal depression (https://www.who.int/publications/i/item/WHO-MSD-MER-15.1)
Scaling-up psychological interventions in resource-poor settings: training and supervising peer volunteers to deliver the ‘Thinking Healthy Programme’ for perinatal depression in rural Pakistan (https://www.cambridge.org/core/journals/global-mental-health/article/scalingup-psychological-interventions-in-resourcepoor-settings-training-and-supervising-peer-volunteers-to-deliver-the-thinking-healthy-programme-for-perinatal-depression-in-rural-pakistan/55A1AE45EFF9BBA944669446ACE8F6F8)
Improving access to psychosocial interventions for perinatal depression in low- and middle-income countries: lessons from the field (https://pubmed.ncbi.nlm.nih.gov/32516019/)
Doing What Matters in Times of Stress (DWMS)
Doing What Matters in Times of Stress (DWMS) serves as a digital, self-guided stress management companion for navigating challenging situations. The guide provides easy to learn skills and audio exercises that can be practiced for just a few minutes each day to help you cope with stress. It is for anyone who experiences stress, wherever they live and whatever their circumstances.
Read more here:
Digital version of “Doing What Matters in Times of Stress” (https://dwmatters.eu/)
Doing What Matters in Times of Stress: An Illustrated Guide (https://www.who.int/publications/i/item/9789240003927)
Doing What Matters in Times of Stress (guide in different languages)(https://www.mhinnovation.net/collaborations/toolkit-integration-mental-health-general-healthcare-humanitarian-settings/doing)
“Doing What Matters in Times of Stress” to Decrease Psychological Distress During COVID-19: A Randomised Controlled Pilot Trial (https://journals.lww.com/invn/fulltext/2022/20020/_doing_what_matters_in_times_of_stress__to.5.aspx)
Highlighting Complementary Benefits of Problem Management Plus (PM+) and Doing What Matters in Times of Stress (DWM) Interventions Delivered Alongside Broader Community MHPSS Programming in Zummar, Ninewa Governorate of Iraq (https://www.researchgate.net/publication/364983127_Highlighting_Complementary_Benefits_of_Problem_Management_Plus_PM_and_Doing_What_Matters_in_Times_of_Stress_DWM_Interventions_Delivered_Alongside_Broader_Community_MHPSS_Programming_in_Zummar_Ninewa_G)
Problem Management Plus (PM+)
Learn more about PM+ with our information leaflet
Problem Management Plus (PM+) is a brief individual or group intervention designed to address psychological or social problems through problem-solving and behavioural interventions. It is delivered through five sessions where participants learn skills to manage stress, solve problems, get active, and strengthen their social support.
Read more here:
PROBLEM MANAGEMENT PLUS (PM+) Individual psychological help for adults impaired by distress in communities exposed to adversity https://iris.who.int/bitstream/handle/10665/206417/WHO_MSD_MER_16.2_eng.pdf?sequence=1
Scaling Up Psychological Interventions with Syrian Refugees (STRENGTHS) (http://strengths-project.eu/en/strengths-home/)
Refugee Minors and Integration (REMAIN) (https://ki.se/en/cns/remain-refugee-minors-and-integration)
RESPOND Project (https://respond-project.eu/)
Ukraine’s displaced people in the EU: Reach out, Implement, Scale-up and Evaluate interventions promoting mental wellbeing (U-RISE) (https://research.vu.nl/en/projects/ukraines-displaced-people-in-the-eu-reach-out-implement-scale-up-)
Building Mental Health and Psychosocial Support Capacity During a Pandemic: The Process of Adapting Problem Management Plus for Remote Training and Implementation During COVID-19 in New York City, Europe and East Africa (https://journals.lww.com/invn/fulltext/2021/19010/building_mental_health_and_psychosocial_support.6.aspx)
After the Randomised Controlled Trial Implementing Problem Management Plus Through Humanitarian Agencies – Three Case Studies from Ethiopia, Syria and Honduras (https://journals.lww.com/invn/fulltext/2021/19010/after_the_randomised_controlled_trial_.11.aspx)
Living Six Hours Away from Mental Health Specialists: Enabling Access to Psychosocial Mental Health Services Through the Implementation of Problem Management Plus Delivered by Community Health Workers in Rural Chiapas, Mexico (https://journals.lww.com/invn/fulltext/2021/19010/living_six_hours_away_from_mental_health.10.aspx)
Psychological First Aid (PFA)
Psychological First Aid (PFA) is an approach to providing initial support and assistance to individuals affected by crises, disasters, or traumatic events. The goal of PFA is to help people cope with the immediate emotional impact of a crisis, reduce initial distress, and foster short-term and long-term adaptive functioning. PFA is not a form of psychotherapy; instead, it focuses on practical and humane support that respects the individual’s dignity, culture, and autonomy. The core principles of PFA include safety, calmness, connectedness, self-efficacy, and hope.
Read more here:
Psychological first aid: Guide for field workers https://www.who.int/publications/i/item/9789241548205
Psychological First Aid Training: A Scoping Review of Its Application, Outcomes and Implementation (https://pubmed.ncbi.nlm.nih.gov/33926108/)
Building mental health and psychosocial support capacity in higher education: psychological first aid training to support displaced Afghan student refugees (http://www.populationmedicine.eu/Building-mental-health-and-psychosocial-support-capacity-in-higher-education-psychological,165410,0,2.html)
Step-by-Step (SbS)
Step-by-Step (SbS) is a five-session, guided, technology-supported intervention specifically designed for depression. Developed by the World Health Organization (WHO), it offers psychoeducation and behavioral activation training through an illustrated narrative and includes diverse therapeutic techniques such as positive self-talk, stress management, and preventing relapse. Step-by-Step is adaptable to diverse cultural contexts and resource settings, ensuring its relevance in communities facing adversity.
Read more here:
Step-by-Step: a new WHO digital mental health intervention for depression (https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6131163/)
Step-by-step: e-mental health in Lebanon (https://www.mhinnovation.net/innovations/step-step-e-mental-health-lebanon )
Effects of a WHO-guided digital health intervention for depression in Syrian refugees in Lebanon: A randomized controlled trial (https://journals.plos.org/plosmedicine/article?id=10.1371/journal.pmed.1004025)
TeamUp
TeamUp is a psychosocial support intervention of structured play, movement, and body awareness activities for children aged 6 to 18 affected by conflict, developed by a coalition of War Child Holland, Save the Children, and UNICEF Netherlands. Trained facilitators use non-verbal, movement-based approaches to ensure the participation of all children, regardless of language barriers. The structured sessions, guided by the principles of ‘same place, same face, same time,’ aim to create a sense of stability and normalcy for the children.
Read more here:
https://www.warchild.net/intervention-teamup/
Process evaluation of TeamUp: a movement-based psychosocial intervention for refugee children in the Netherlands (https://ijmhs.biomedcentral.com/articles/10.1186/s13033-021-00450-6)
Case Study: TeamUp Netherlands – From theory of change to implementation (https://www.unicef-irc.org/files/documents/d-4195-38925-CS5-TeamUp%20Netherlands-vis05r1.pdf)
BeThere

The BeThere intervention directly addresses the psychosocial wellbeing of parents and caregivers – in addition to developing positive parenting techniques. The nine-session programme sees small groups of caregivers meet for sessions conducted by trained facilitators – with the overall aim of reducing stress and improving psychosocial wellbeing.
Read more here:
War Child Holland website on BeThere (https://www.warchild.net/intervention-bethere/)
Supporting Syrian families displaced by armed conflict: A pilot randomized controlled trial of the Caregiver Support Intervention (https://pubmed.ncbi.nlm.nih.gov/32408022/)
ReachNow
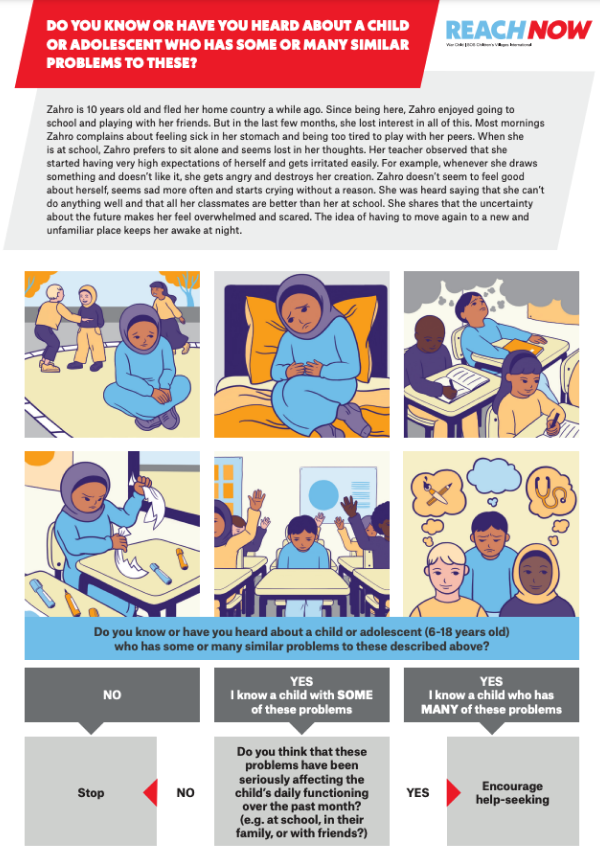
The ReachNow tool, developed by War Child Holland, aims to improve help-seeking among children and adolescents in need of mental healthcare by strengthening community-level proactive detection and help-seeking encouragement. The tool is made up of illustrated vignettes depicting most common, culturally relevant indicators of childhood psychological distress as well as decision-making diagrams, to guide community members and lay people towards seeking further support, if necessary.
Read more here:
WarChild Holland website on ReachNow (https://www.warchild.net/intervention-reachnow/)
ReachNow detection tool (https://www.warchild.net/documents/262/220420_WCH_REACHNOW_CO-BRANDING_DETECTION_TOOL_EN.pdf)
Accuracy of a Proactive Case Detection Tool for Internalizing and Externalizing Problems Among Children and Adolescents (https://www.researchgate.net/publication/353369281_Accuracy_of_a_Proactive_Case_Detection_Tool_for_Internalizing_and_Externalizing_Problems_Among_Children_and_Adolescents)
Early Adolescent Skills for Emotions (EASE)
Early Adolescent Skills for Emotions (EASE) is an evidence-based group psychological intervention to support 10–15-year-olds facing internalizing problems (such as stress, anxiety, and depression symptoms) in communities affected by adversity. The intervention comprises seven group sessions for adolescents, along with three additional group sessions tailored for their caregivers, and aims to equip adolescents and their caregivers with skills to alleviate distress. Drawing from adapted elements of Cognitive Behavioral Therapy, EASE is designed for delivery by trained and supervised non-specialist helpers.
Read more here:
Early Adolescent Skills for Emotions (EASE) (https://iris.who.int/bitstream/handle/10665/374996/9789240082755-eng.pdf?sequence=1)
Implementing a Non-Specialist Delivered Psychological Intervention for Young Adolescents in a Protracted Refugee Setting: a Qualitative Process Evaluation in Lebanon (https://pubmed.ncbi.nlm.nih.gov/38087061/)
Cultural adaptation of a scalable psychological intervention for Burundian refugee adolescents in Tanzania: a qualitative study (https://conflictandhealth.biomedcentral.com/articles/10.1186/s13031-021-00391-4)
mhGAP

The Mental Health Gap Action Programme (mhGAP) is an initiative of the WHO aimed at scaling up care for mental, neurological, and substance use disorders. The goal of mhGAP is to address the significant gap that exists globally between the need for mental health services and the availability of those services, especially in low- and middle-income countries. The mhGAP intervention guide provides a framework for the management of priority mental, neurological, and substance use disorders in non-specialized health care settings.
Read more here:
mhGAP Intervention Guide – Version 2.0 (https://www.who.int/publications/i/item/9789241549790)
Psychosocial support during childbirth: Development and adaptation of WHO’s Mental Health Gap Action Programme (mhGAP) for maternity care settings (https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0285209)
Considering culture, context and community in mhGAP implementation and training: challenges and recommendations from the field (https://ijmhs.biomedcentral.com/articles/10.1186/s13033-019-0312-9)
Enhancing mental health pre-service training with the mhGAP Intervention Guide: experiences and lessons learned (https://www.who.int/publications/i/item/9789240007666)
Narrative Exposure Therapy (NET)

Narrative Exposure Therapy (NET) is a universally applicable, human-rights focused, evidence-based treatment for child-, adolescent- and adult survivors of multiple and complex trauma. Within a life-span approach, NET enables the integration of traumatic memories into the autobiographical context, activates the person’s resources, and allows meaning-making and corrective relationship experiences. NET is distinct from other treatments in its explicit focus on recognising and creating a testimony of what happened in a way that serves to recapture the patient’s self-respect and acknowledges the abuse of their human rights that has taken place. There are various efficacious modules of Narrative Exposure Therapy: ‘NET’ in its classic, universal form, ‘KIDNET’ which builds on classic NET with an adaptation for children and youth, FORNET with a special focus on perpetrating clients suffering from Appetitive Aggression, NETfacts a community-based module, developed for the rehabilitation of entire communities that have been struck by trauma.
Read more here:
https://www.net-institute.org/
NETfacts: An integrated intervention at the individual and collective level to treat communities affected by organized violence
https://www.pnas.org/doi/abs/10.1073/pnas.2204698119
Systematic review and meta-analyses of the long-term efficacy of narrative exposure therapy for adults, children and perpetrators https://www.tandfonline.com/doi/abs/10.1080/10503307.2020.1847345
Adapting narrative exposure therapy with a tribal community: A community-based approach (https://pubmed.ncbi.nlm.nih.gov/35621371/)
Feasibility of narrative exposure therapy in an outpatient day treatment programme for refugees: improvement in symptoms and global functioning (https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7473203/)
Impact and cultural acceptance of the Narrative Exposure Therapy in the aftermath of a natural disaster in Burundi (https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6052646/ )

For us, capacity strengthening refers to all the activities involved in building on existing capacities in your organization and team members, so you can deliver scalable MHPSS interventions and approaches confidently, effectively, and safely. This includes the knowledge and skills needed for effective and sustainable programme and project planning and management and ensuring the integration of scalable interventions into your existing work is done ethically and sustainably. It includes training your trainers, who can, in turn, train facilitators on how to deliver the interventions, with practical application under close supervision as part of the training. It also includes opportunities for research and follow-up support to ensure you are on the right track with delivery of the interventions.
One of our key assets is our strong relationships with academic institutions worldwide who are working with and researching scalable psychological interventions. They help us to develop quality assurance tools and continually reflect on our capacity strengthening methods to improve them.